Malaria - All you need to know
GS-3 Science and Technology
Introduction
Malaria is a life-threatening mosquito-borne disease that affects millions of people worldwide, especially in tropical and subtropical regions. It is caused by the Plasmodium parasite and transmitted through the bites of infected female Anopheles mosquitoes.
In this comprehensive guide, we will delve into the intricate details of malaria, exploring its causes, symptoms, prevention, and the complex life cycle of the malarial parasite.
Understanding the Disease
Malaria is caused by five species of the Plasmodium parasite, with Plasmodium falciparum being the most dangerous and responsible for severe malaria cases. The parasite enters the human bloodstream through the bite of an infected mosquito and travels to the liver, where it multiplies before infecting red blood cells. Once inside the red blood cells, the parasite replicates and leads to the characteristic cyclic symptoms of malaria.
Causes and Transmission
Malaria transmission occurs through the bite of infected female Anopheles mosquitoes. These mosquitoes carry the Plasmodium parasite in their salivary glands and transmit it to humans during a blood meal. Factors such as stagnant water, high humidity, and warm temperatures contribute to increased mosquito breeding and, consequently, higher malaria transmission rates.
Signs and Symptoms
Malaria symptoms typically manifest 10-15 days after an infected mosquito bite. The classic symptoms include high fever, chills, sweats, headaches, and body aches. In severe cases, malaria can lead to organ failure, anemia, and even death. Prompt diagnosis and treatment are crucial to preventing severe complications.
Diagnosing Malaria
Accurate and timely diagnosis is vital for effective malaria management. Microscopic examination of blood smears is the gold standard for malaria diagnosis, where trained technicians identify the presence of Plasmodium parasites in blood samples. Rapid diagnostic tests (RDTs) are also available, providing quicker results and enabling timely treatment.
The Life Cycle of the Malarial Parasite
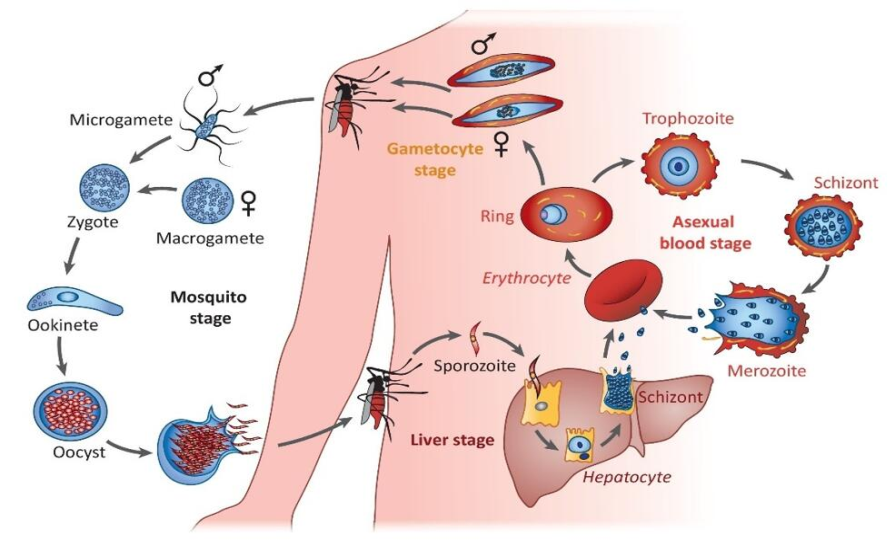 The life cycle of the malarial parasite, primarily belonging to the Plasmodium species, is complex and involves two hosts: humans and female Anopheles mosquitoes. There are five species of Plasmodium that cause malaria in humans, with Plasmodium falciparum being the most lethal. Here is a detailed explanation of the malarial parasite's life cycle:
The life cycle of the malarial parasite, primarily belonging to the Plasmodium species, is complex and involves two hosts: humans and female Anopheles mosquitoes. There are five species of Plasmodium that cause malaria in humans, with Plasmodium falciparum being the most lethal. Here is a detailed explanation of the malarial parasite's life cycle:
- Transmission to Humans: Infected female Anopheles mosquito bites humans, injecting sporozoites into the bloodstream.
- Liver Stage (Exoerythrocytic Schizogony): Sporozoites reach the liver, infect hepatocytes, undergo asexual reproduction, forming merozoites.
- Release and Invasion of Red Blood Cells: Mature merozoites leave the liver, invade red blood cells.
- Intraerythrocytic Development: Merozoites develop into ring-shaped trophozoites, multiply, cause fever and chills.
- Cyclic Nature of Symptoms: Periodic release and invasion of red blood cells cause recurring symptoms with varying periodicity.
- Gametocyte Formation: Some merozoites become sexual forms (gametocytes) for mosquito transmission.
- Transmission to Mosquito: Infected mosquito feeds, ingesting gametocytes and asexual parasites.
- Fertilization and Sporogony: Gametes fertilize, forming sporozoites within the mosquito's gut.
- Migration to Salivary Glands: Sporozoites move to salivary glands, become infectious. Next bite transmits sporozoites, starting the cycle again.
Understanding the intricate life cycle of the malarial parasite is crucial for developing effective strategies to control and prevent the spread of malaria. Researchers and healthcare professionals continue to study the parasite's biology to develop better diagnostic tools, treatments, and vaccines, with the ultimate goal of eradicating malaria globally.
Preventive measures
Preventing malaria is essential to reduce its impact on public health. Several preventive measures can be taken, such as:
- Using mosquito nets treated with insecticides to protect against mosquito bites.
- Applying insect repellents to exposed skin when in mosquito-infested areas.
- Eliminating mosquito breeding sites by draining standing water and maintaining clean surroundings.
- Preventive chemotherapy involves using medicines, alone or in combination, to prevent infections and their effects. It includes various approaches like chemoprophylaxis, intermittent preventive treatment for infants and pregnant women, seasonal malaria chemoprevention, and mass drug administration. These strategies are safe and cost-effective and work alongside other control measures like vector control, early diagnosis, and treatment of malaria cases with antimalarial drugs. The goal is to enhance the effectiveness of malaria control efforts and reduce the burden of the disease.
Treatment and Management of Malaria
The treatment of malaria depends on the species of Plasmodium and the severity of the infection. The treatment of malaria involves the use of antimalarial medications to clear the malaria parasite from the bloodstream and cure the infection.
Commonly used drugs include Artemisinin-based Combination Therapies (ACTs) for uncomplicated malaria and severe cases, Quinine for severe malaria, and Primaquine to prevent relapses of certain malaria species. Prompt medical attention is crucial for early diagnosis and effective treatment. Early detection and appropriate antimalarial therapy can prevent complications and improve outcomes. It is essential to follow healthcare professional guidance and complete the full course of treatment to ensure successful recovery.
Malaria Vaccine
In 2020, the World Health Organization (WHO) endorsed the first antimalarial vaccine called
RTS, S/AS01 (Mosquirix). Developed by GlaxoSmithKline (GSK), it is recommended as part of the E-2025 initiative to combat malaria. The vaccine, used alongside existing tools, could save thousands of young lives annually. WHO based its recommendation on results from pilot programs in Ghana, Kenya, and Malawi. Malaria remains a significant cause of childhood illness and death in sub-Saharan Africa, with over 260,000 African children under five dying from the disease each year. World Malaria Day, observed on April 25th, aims to raise awareness and fund research for eradication. The WHO has identified 25 countries for potential malaria eradication by 2025 under the 'E-2025 Initiative'.
India and Malaria
Key highlights of recent WHO report
-
WHO World Malaria Report 2020: India continues to make Impressive Gains in reduction of Malaria Burden
-
India the only high endemic country which has reported a decline of 17.6% in 2019 over 2018
-
India has sustained Annual Parasitic Incidence (API) of less than one since 2012
According to the World Malaria Report (WMR) 2020 released by the WHO, India has made significant strides in reducing its malaria burden. As the only high endemic country, India reported a remarkable 17.6% decline in malaria cases in 2019 compared to 2018. The Annual Parasitic Incidence (API) also reduced by 27.6% in 2018 compared to 2017 and by 18.4% in 2019 compared to 2018, sustaining API less than one since 2012.
India's efforts have contributed to the largest drop in cases in the region, witnessing a substantial decrease from around 20 million to about 6 million cases. Over the period of 2000 to 2019, the percentage drop in malaria cases was 71.8%, and in deaths, it was 73.9%.
Remarkably, India achieved an impressive 83.34% reduction in malaria morbidity and a remarkable 92% reduction in malaria mortality between 2000 (20,31,790 cases, 932 deaths) and 2019 (3,38,494 cases, 77 deaths), successfully accomplishing Goal 6 of the Millennium Development Goals, aiming for a 50-75% decrease in case incidence between 2000 and 2019.
Epidemiological trends of Malaria in India (2000-2019) Pv; Plasmodium Vivax & pf; Plasmodium Falciparum
Malaria cases in India have shown a consistent decline. In 2019, there was a 21.27% reduction in cases (3,38,494) and a 20% decrease in fatalities (77 deaths) compared to 2018 (4,29,928 cases, 96 deaths). The trend continued in 2020, with reported cases decreasing by 45.02% (1,57,284) until October, compared to the same period in 2019 (2,86,091).
India initiated malaria elimination efforts in 2015, and with the launch of the National Framework for Malaria Elimination (NFME) in 2016 by the Ministry of Health and Family Welfare, the fight against malaria gained momentum. To further strengthen the efforts, the Health Ministry introduced the National Strategic Plan for Malaria Elimination (2017-22) in July 2017, outlining comprehensive strategies for the next five years.
Epidemiological situation of Malaria in India (2015 – 2019)
In the initial two years, there was a substantial decline in malaria cases and fatalities in India, showing a reduction of 27.7% in cases (from 11,69,261 in 2015 to 8,44,558 in 2017) and 49.5% in fatalities (from 385 deaths in 2015 to 194 deaths in 2017).
Certain states, namely Odisha, Chhattisgarh, Jharkhand, Meghalaya, and Madhya Pradesh, accounted for approximately 45.47% (1,53,909 cases out of India's total of 3,38,494 cases) of malaria cases and 70.54% (1,10,708 cases out of India's 1,56,940 cases) of falciparum malaria cases in 2019. Additionally, these states reported 63.64% (49 out of 77) of malaria-related deaths in the country.
India's efforts to combat malaria include providing microscopes, rapid diagnostics, and distributing Long-Lasting Insecticidal Nets (LLINs). Around 5 crores of LLINs were distributed in 7 North-East States, Chhattisgarh, Jharkhand, Madhya Pradesh, and Odisha till 2018-19, with an additional 2.25 crore LLINs supplied this year in high-burden areas. An additional procurement of 2.52 crore LLINs has been initiated. The community widely accepts LLINs, contributing significantly to the decline in malaria cases.
India's engagement in the WHO's HBHI initiative showed impressive outcomes: 18% fewer malaria cases and 20% fewer deaths in the last two years. Making malaria notifiable in 31 states/UTs, including high-endemic areas, like Odisha, Meghalaya, Jharkhand, Madhya Pradesh, and Chhattisgarh, led to significant case reductions. With strategic interventions, India aims to achieve the 2030 malaria elimination target.
GIS maps – Shrinking malaria endemicity (District level)
India's National Strategic Plan (NSP) for Malaria Elimination has set key objectives to combat the disease:
- Ensure universal coverage of case detection and treatment services in endemic districts, aiming for 100% parasitical diagnosis and complete treatment of all confirmed malaria cases.
- Enhance the surveillance system to detect, notify, investigate, classify, and respond to all cases across all districts, driving towards total malaria elimination.
- Implement appropriate vector control interventions to achieve near-universal coverage of the population at risk of malaria.
- Focus on effective program management and coordination at all levels, employing targeted interventions for malaria elimination.
While malaria was nearly eradicated in India, it resurged in the 1970s, with around 1.5 million cases, predominantly caused by the deadly Plasmodium falciparum parasite, reported in 2009. The NSP represents the Union Health Ministry's first comprehensive roadmap to eliminate the disease. Achieving the 2027 elimination targets may pose challenges, but strong political commitment and a focused approach can drive progress. While diseases like malaria, HIV-AIDS, and tuberculosis have gained attention and funding for research and treatment, other neglected diseases affecting impoverished communities require similar focus and support.
Way forward
Malaria remains a significant public health challenge in India, affecting millions of people across the country. To effectively manage this disease, it is crucial for India to understand its causes, symptoms, prevention, and treatment options. Combating malaria demands a comprehensive approach, involving coordinated efforts from the Indian government, healthcare professionals, local communities, and individuals.
- Research-driven strategies to combat malaria effectively
- Tailored interventions for regional challenges
- Implementing preventive measures like mosquito nets, indoor spraying, and chemoprophylaxis
- Controlling mosquito populations through environmental measures
- Individual responsibility in adopting protective measures
- Supporting community initiatives for prevention programs
- Public awareness campaigns for early detection and prompt medical attention
- Adequate funding and strong healthcare infrastructure for malaria control
- Ensuring access to affordable and quality antimalarial drugs and diagnostic tools.
In conclusion, eradicating malaria in India requires a concerted effort from all stakeholders involved. Through research, customized preventive measures, heightened public awareness, and strong governmental commitment, India can make significant strides in curbing the spread of malaria and saving countless lives. By working together, we can envision a future where malaria is no longer a burden on the Indian population, and the country can thrive free from this disease.