GS Paper II
News Excerpt:
Recently, a study done by researchers about the healthcare centers in 5 North Indian States showed a pattern of improving quality and utilisation over time but the nature of progress is largely cosmetic and the pace is slow.
Why do health centres matter?
- Economic Survey 2022-23 showed that in the absence of proper insurance and affordable services, almost half of all health spending in India is still paid by patients themselves, pushing many households into poverty.
- Health centres are at the bottom of the health chain of India’s public health system, charged with offering accessible and affordable primary care.
- Almost two lakh in number, they are conceptualised as a three-tier system:
-
- Sub-centres (later renamed as health and wellness centres)
-
- Public health centres (PHCs) and
-
- Community health centres (CHCs)
- 94% of these centres are located in rural areas, but reports show that less than 20% of them function effectively, pushing disadvantaged communities to rely on expensive, exploitative private health care.
Key findings of the study:
- The researchers studied the performance of 241 health centres — 26 CHCs, 65 PHCs and 150 sub-centres, spread across Bihar (23), Chhattisgarh (36), Himachal Pradesh (45), Jharkhand (37) and Rajasthan (100).
- Himachal Pradesh has been a pioneer with functional centres serving 83% of its population, but States like Chhattisgarh and Rajasthan have introduced valuable initiatives.
- Health centres today have better facilities, dispense more medicines, serve more patients, and provide a wider range of services than they did 10 or 20 years ago.
- Health workers too agree that the work environment and the work culture seem to improve together.
|
Case Studies:
|
- What changed between 2002 and 2022?
- The share of health expenditure in the Union Budget increased drastically, coupled with the introduction of the National Rural Health Mission.
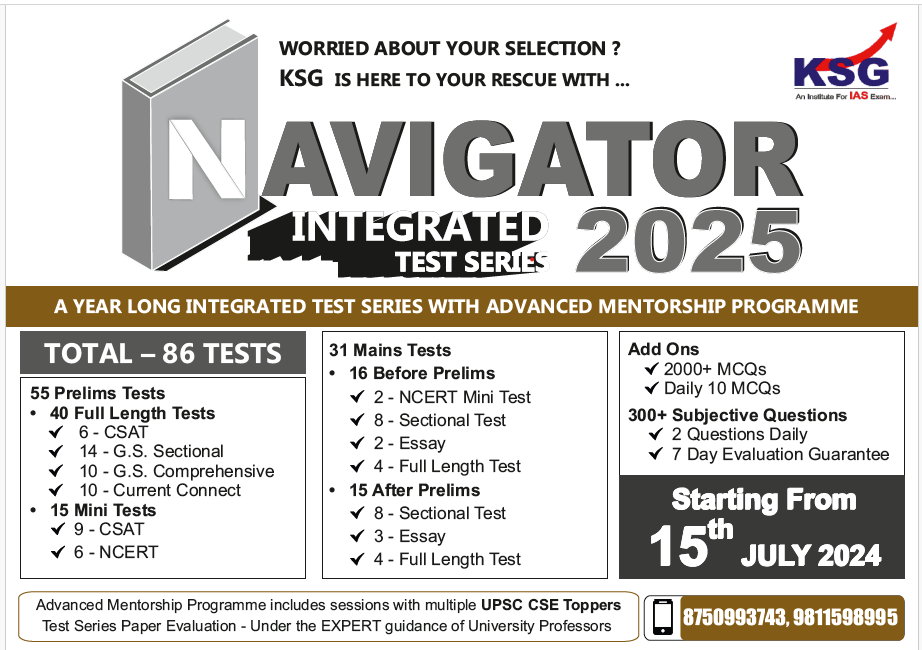
- India’s flagship Ayushmann Bharat programme, launched with the vision of achieving universal health coverage, in 2018 introduced a health insurance component (PMJAY) and a public provision component through health and wellness centres (HWCs).
- State-specific schemes launched by Rajasthan and Chhattisgarh boosted their performance.
- The survey noted that COVID-19 contributed to a “sustained increase in patient utilisation”, with people placing greater trust in public health facilities.
- The health centres are still “grossly underutilised”: there is high staff absenteeism, the number of patients per day is low, services are limited and of poor quality.
- The health workers also pointed to some of the drawbacks like: - lack of staff ; irregular flow of funds; lack of toilet facilities; no transport or residential facilities; no drugs or functional testing equipment; and the growing burden of both online and on-field work.
- The study also documented social discrimination in health centres: some upper-caste doctors had “disparaging attitudes towards marginalised communities”, and upper-caste families routinely disrespected Dalit ANMs.
- ANMs and ASHAs worked in grim environments with centres lacking running water and toilets.
|
Ayushman Bharat:
|
Investments in Healthcare:
- Investment in healthcare increased, but the “improvements are patchy” and allocations prioritise material development in tertiary healthcare.
- According to the composition of the healthcare budget: the allocation in 2022–23 (1.9%) was almost the same as a decade ago in 2013–14 (1.7%).
- The National Health Mission share shrank from 69% to 44%.
- The government spent 10 times as much money on PMJAY and new regional AIIMS hospitals than on public welfare arms like the Health wellness centres (HWCs).
- The HWCs have a relatively attractive look but were only marginally better than sub-centres, with improvements only “cosmetic” in nature.
Way forward: It is imperative to address the existing challenges and gaps in the healthcare system to ensure equitable access to quality healthcare for all. This can be achieved through several key strategies:
- Strengthening Primary Health Care: Focus on enhancing the capacity and infrastructure of primary healthcare centers (PHCs) and sub-centers, especially in states like Bihar, to improve their quality and effectiveness in delivering essential healthcare services.
- Improving Quality of Services: Ensure availability of essential medicines, diagnostic equipment, and basic facilities like running water and toilets at all health centers to enhance the quality of services.
- Enhancing Community Participation: Encourage community participation in healthcare delivery through the involvement of Accredited Social Health Activists (ASHAs) and community health workers to bridge the gap between healthcare providers and communities.
- Monitoring and Evaluation: Establish robust monitoring and evaluation mechanisms to track the progress of healthcare initiatives and ensure accountability in the delivery of healthcare services.
Conclusion:
The researchers conclude by noting that “beyond the current tokenism of Ayushmann Bharat”, “major support from the centre would make it much easier for the poorer states to emulate these initiatives”.