Tackling the fatty liver disease epidemic
Relevance: GS Paper I & II
Why in News?
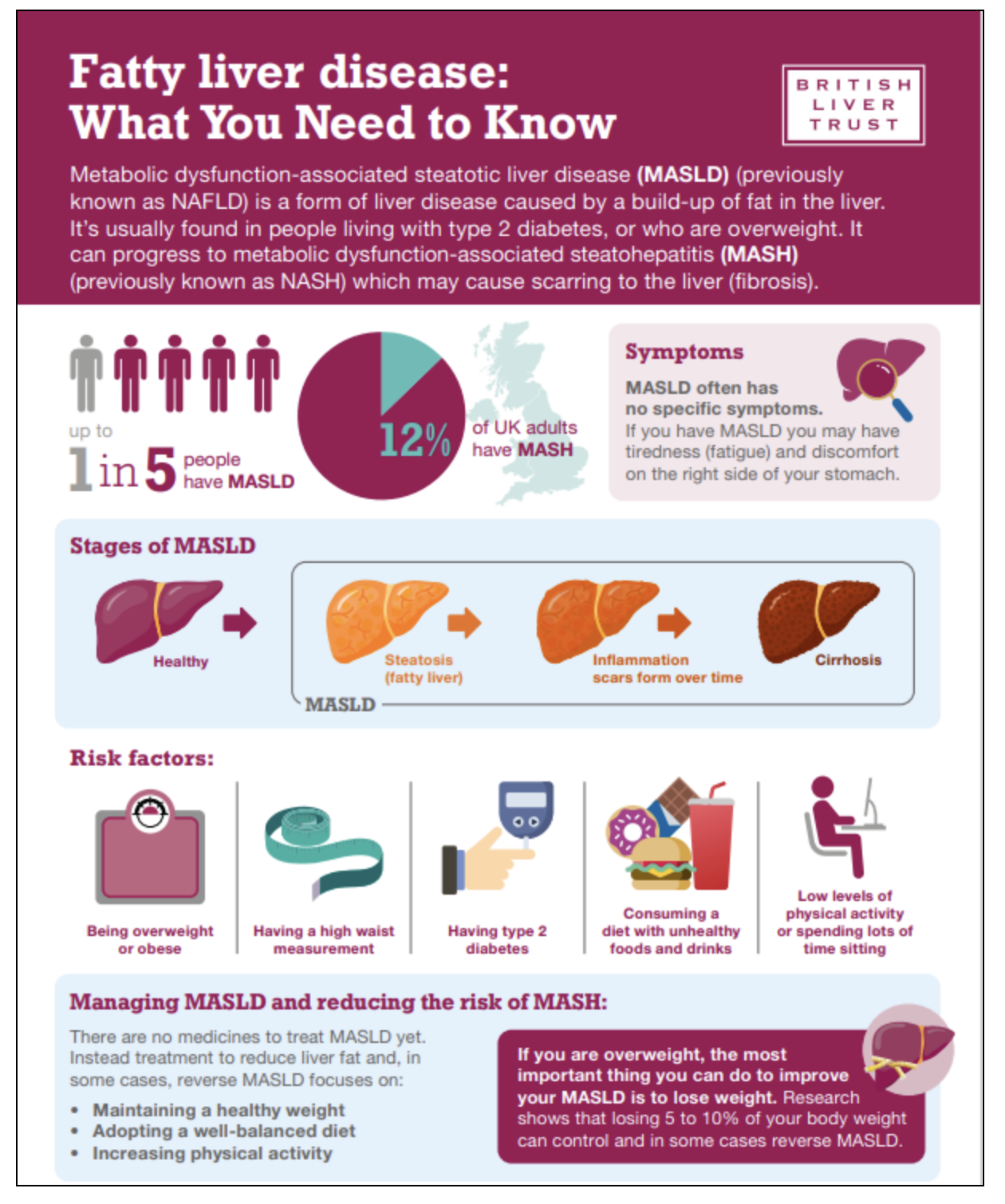
There is a close link between fatty liver disease and metabolic syndrome, including obesity, diabetes, high blood pressure, and abnormal cholesterol levels.
About the news:
- The theme for International Fatty Liver Day this year is ‘Act Now, Screen Today’.
- Liver diseases were predominantly associated with excessive alcohol use and this remains an important cause of advanced chronic liver disease.
- However, in recent years, there has been the emergence of a silently growing threat to liver health — non-alcoholic fatty liver disease.
- Fatty liver is closely linked to metabolic health, cardiac health, and a risk for developing cancers.
- This disorder has now been appropriately reclassified and is known as ‘Metabolic dysfunction-associated steatotic liver disease’ (MASLD).
- The new nomenclature MASLD, replaced the previously used term NAFLD (non-alcoholic fatty liver disease) to encompass a broader number of steatosis types.
- It has also resulted in a paradigm shift in how we approach liver health.
- The key is to screen, test, and treat.
Growing burden:
- The trends in fatty liver disease prevalence are alarming.
- MASH (Metabolic dysfunction-associated steatohepatitis), a progressive form that causes liver inflammation and scarring, is expected to become the most common cause of chronic liver disease and the leading indication for liver transplantation.
- The global prevalence of MASLD is estimated at 25-30%.
- In 2022, a meta-analysis revealed that in India, among adults, the pooled prevalence of fatty liver was 38.6%, while among obese children, it was around 36%.
- There is a close link between fatty liver disease and metabolic syndrome, including obesity, diabetes, high blood pressure, and abnormal cholesterol levels.
- Individuals with these conditions have high MASLD prevalence rates:
- 55.5%-59.7% for diabetes,
- 64.6%-95% for obesity, and
- 73% for severe metabolic syndrome.
- Individuals with these conditions have high MASLD prevalence rates:
- The process leading to the fatty liver:
- Consuming excessive carbohydrates worsens these conditions by causing metabolic problems.
- When the body has too much glucose, it increases insulin production to help cells absorb the glucose. However, constantly eating too many carbs causes persistently high insulin levels, leading to insulin resistance.
- Insulin resistance disrupts normal metabolism and promotes the conversion of excess glucose into fatty acids, which are then stored in the liver. The liver cells fill up with fat, leading to fatty liver.
- Over time, this continuous damage affects the liver’s ability to function properly, progressing from simple fatty liver to more severe conditions such as steatohepatitis and cirrhosis, which are hallmarks of MASLD and may require a liver transplant.
- Fatty liver disease often goes undetected as there is usually no warning or symptom in the early stages.
- Diagnosis is usually made at an advanced stage, often when significant liver damage has already occurred.
- The key to early diagnosis is a comprehensive health screening that includes:
- Thorough history
- Physical examination: height, weight, body mass index (BMI), abdominal girth, and waist-to-hip ratio to assess visceral fat.
- Blood tests: a blood count, sugar profile, blood lipid profile, liver function tests, and kidney tests.
- Ultrasound of the abdomen: It is often missed or not included in many health checks, largely because of the limited availability of radiologists and stringent regulatory approvals.
- Advanced liver tests will include liver fibrosis assessment to look for liver scarring, done by using newer technologies such as vibration-controlled transient elastography.
- Together, these tools — ultrasound, comprehensive metabolic screening, and elastography — form an integrated approach to detect and manage liver diseases at an early stage effectively.
Way Forward:
- Effective management of fatty liver diseases hinges on a multidisciplinary collaborative approach that harnesses the collective expertise of healthcare providers, researchers, policymakers, and advocacy groups.
- Comprehensive awareness and education strategies are the cornerstones in the battle against this disease, empowering individuals to take charge of their health and thwart disease progression.
- While the Ministry of Health and Family Welfare, Government of India, advocates for public-private partnerships to be integrated with other programs to monitor and evaluate liver diseases, the healthcare industry must lead the charge and confront the silent threat of liver diseases.
- The selection of screening tests and the frequency with which they are performed should be personalised and based on factors including an individual’s risk factors such as family history, lifestyle, and pre-existing health conditions.
- Clinicians should not make generic assumptions given the patient’s age or physical markers alone as we are increasingly witnessing non-communicable diseases break traditional stereotypes and impact very diverse people.
- There is a need for integrated strategies that combine dietary modifications, regular physical activity, and effective weight management to mitigate liver disease risks.
Conclusion:
The liver is a ‘silent organ’ that typically does not exhibit noticeable signs of damage until it reaches an advanced stage. Thus, we need to take active control of our health, be aware of what we consume, and go for frequent screenings.